
Reda Hamdi, Laura Tissot, Christophe Guichard, Patrick Manipoud
ENT department of the metrople savoie regional hospital Hôpital de Chambéry, Place Lucien Biset, Fbg Maché, 73000 Chambéry, France.
*Corresponding author: Reda Hamdi, ENT department of the metrople savoie regional hospital Hôpital de Chambéry, Place Lucien Biset, Fbg Maché, 73000 Chambéry, France.
Received: March 29, 2023
Accepted: April 03, 2023
Published: April 10, 2023
Citation: Hamdi H, Tissot H, Guichard C, Manipoud
P. (2023) “Case Report: Double Gingival Metastasis of Hepatocellular Carcinoma”, Clinical Oncology Case Reports and Research, 1(1); DOI: http;//doi.org/04.2023/1.1001.
Copyright: © 2023 Reda Hamdi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article reports a case of gingival metastasis of hepatocellular carcinoma (HCC) in a 70-year-old Asian patient. The patient presented with a painful, rapidly growing gingival mass that was ultimately diagnosed as a metastasis of HCC. This case highlights the importance of considering metastatic disease as a differential diagnosis when evaluating oral lesions, particularly in patients with a history of cancer. The article also discusses the possible mechanisms and routes of metastasis of HCC to the gingiva, as well as the treatment options for this rare manifestation of HCC.
Introduction
Hepatocellular carcinoma (HCC) is France's second leading cause of digestive cancer. It represents 0.5 to 2% of all cancers, with approximately 6,000 new cases annually in France. HCC occurs in cirrhotic livers in more than 85% of cases, mainly of alcoholic or viral origin[1]. Most patients are male (male to female ratio, 46:4) and over 50 years old in 90% of cases [2]. Extrahepatic metastases occur in 25 to 37% of cases [3;4].cases and preferentially involve the lungs, regional lymph nodes, locomotor adrenal glands, and rarely the oral region [5;6].
Oral metastases of HCC are present in 30% of cases before discovering primary cancer [7]. The mandibular bone is most often affected [8]. Gingival metastases are rare [6, 9]. When present, it is often associated with other localizations, particularly pulmonary [10].
Narrative
The case presented is a new case of gingival metastasis of a mandibular HCC occurring in a 70-year-old woman from China who speaks only Chinese, She was hospitalized in the department of gastroenterology and digestive oncology and addictology of the metropole Savoie hospital of Chambéry for chemotherapy for hepatocellular carcinoma in evolutive pursuits on autoimmune cirrhosis with iterative punctures of the ascites liquid within the framework of peritoneal carcinoids. It should be remembered that the patient was treated for a recurrent uni-focal hepatocellular carcinoma by segmentectomy of segment VII at the University Hospital of Grenoble Alps whose anatomopathological results had found a low differentiated hepatocellular carcinoma of EDMONSON grade III.
The treatment was completed by chemotherapy at the hospital of Chambéry in August 2021, following an evolutive pursuit, and during its follow-up, the patient was very asthenic very painful at the oral level, and presented a mass at the level of the gingival lower labial level, in front of the incisors, rounded and pediculated, well limited, purplish red, bleeding on contact, slightly overflowing extra buccal, very painful, preventing feeding, suggesting a botriomycoma of the gum (figure 1)
The rest of the examination of the oral cavity shows a rather precarious oral and dental condition, the oral mucosa, jugal, and tongue were without particularity, tonsils, and pharynx also.
The rest of the ENT examination, especially rhinological and otological
The nasofibroscopy was also normal

Figure 1: mage showing the gingival metastatic tumor. A reddish and friable gingival mass, originating on both sides of the lower gingiva opposite the insertion of the incisors
Patient Perspective
The patient underwent a biopsy, under local anesthesia, during the same consultation time While waiting for the results, the patient continued her palliative treatment with chemotherapy
After one week, the results came back in favor of a gingival metastasis of her HCC Histological examination revealed a neoplasm covered with squamous epithelium interspersed with cells developed in an invasive trabecular pattern surrounded by a sinusoidal network. Broadly resembling hepatocytes, the tumor cells with abundant cytoplasm showed moderate nuclear atypia with few discernible nuclei (Fig. 2). This microscopic appearance was consistent with the diagnosis of HCC. Immunohistochemistry (IHC) supplements showed that the tissue had strong positive reactions to antibodies against hepatocytes, CAM5, and CD10 and low affinity for antibodies against glypican-3, arginase -1, thyroid transcription factor-1, and cytokeratin-7. Finally, the gingival mass was definitively diagnosed as a metastasis of HCC.
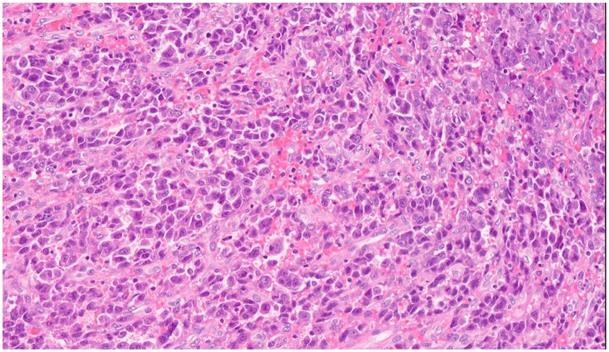
Figure 2: histopathological section. Hematoxylin and eosin stain showing oral squamous mucosa with submucosal proliferation of malignant epithelioid cells arranged in a trabecular architecture. The tumor cells are similar to hepatocytes with moderate nuclear atypia and abundant cytoplasm.
Discussion
According to a large-scale global cancer survey [11], hepatocellular carcinoma (HCC) ranks sixth in global cancer incidence and fourth in cancer mortality. Despite significant reductions in mortality in East Asian countries such as China, South Korea, and Japan, HCC remains the third most common and deadliest cancer. More than 50% of HCC patients have extrahepatic metastases, most commonly involving the lungs, bones, brain, and abdominal lymph nodes [12]. HCC metastases to the gum are considered extremely rare. However, the rarity of gingival metastases may be overestimated; some cases published in English [6, 13,14] or non-English literature [7, 15] journals have not been included in the major databases of the literature. Some cases may not have been reported at all because of potential misdiagnosis. Not all cases are reported because some may be misdiagnosed. Misdiagnosis often occurs when cases have only gingival lesions [7, 14, 16, 17, 18, 19]. There are cases where it is mistaken for gingival begnine disease [3, 20], which leads to even more misdiagnosis, especially if there is no biopsy or pathological examination.
Gingival metastasis can originate from a variety of primary sites, including lung, breast, kidney, bone, colon, adrenal gland, and liver [21]. The possible pathophysiological mechanism of HCC metastasis to the gingiva remains to be elucidated. Invasion of branches of the hepatic artery or portal vein is the preferred mode of oral metastasis [22-23], although metastatic lung tumors are absent in some cases [11, 14,19,24-25, 26-27 , 28 , 29, , 30, 31, 32]. In these cases, the valveless vertebral venous plexus (Batson plexus) has been proposed as a mechanism to bypass filtration of the pulmonary, inferior vena cava and portal circulation [33,34]. This pathway may be the most likely to lead to HCC metastasis to the gingiva without pulmonary metastasis. In addition to the Batson plexus, other possible pathways for gingival metastasis include the arterial, venous, and lymphatic circulation [35]. Given that cirrhosis occurs in more than 50% of HCC patients with metastatic gingival tumors, we cautiously elevate the hypothesis that hemodynamic alteration due to esophageal
varices may be one of the pathways for oral metastasis, especially in patients with HCC on cirrhotic liver with incomplete compensation.
At least 30 cases of gingival HCC metastasis have been collected from existing literature resources. Analysis of these cases can help us better understand the clinical and pathologic features of gingival HCC metastases. First, our current analysis suggests that there is a significant sex preference in the occurrence of gingival HCC metastasis. The male- to-female ratio is greater than 6:1 (26:5), far exceeding the overall male-to-female ratio of approximately 3:1 in liver cancer incidence [11]. These inconsistencies raise the question of whether relatively poor general health habits or oral health behaviors (such as smoking and alcohol consumption) in men, as revealed in one study [36], promote gingival HCC metastases. The pathogenesis of this particular metastasis is thought to be related to oral inflammation, such as gingivitis, which eventually attracts cancer cells to migrate and adhere to the gum [23]. Chronic inflammation is involved in various stages of tumorigenesis, including cell transformation, survival, proliferation, invasion, angiogenesis and metastasis [37,38]. The rich capillary network of chronically inflamed gingiva and the presence of certain inflammatory molecules may promote the progression of metastatic cells [23]. Further research on this possible mechanism remains to be done.
Additionally, an analysis of survival data revealed that patients who initially displayed a gingival mass as a sign of HCC had a very low survival rate. This inaccurate assessment of survival may have been caused by concurrent numerous extra hepatic metastases.
Nevertheless, there have only been three reports of distant metastases outside the gingiva among HCC cases with gingival lesions as the primary symptom [16, 19, 39]. In this scenario, the survival may be made worse by the delay in diagnosis and treatment, which is partially due to the lack of subjacent liver cancer symptoms. This highlights the significance of early diagnosis and treatment of any potential gingival metastases from HCC or other distant tumors. Even if a tumor looks similar, a timely biopsy is required.
Moreover, the HCC is more likely to spread to the upper gingiva than the lower one. We discover several structural factors for this diffusion preference by studying the anatomy. The anatomical features of the gingival arteries that irrigate them may make a difference. The upper respiratory tract's two main blood vessels—the sub-orbital and dental upper arteries— take in blood. The two arteries have larger diameters and larger volume of blood as they are directly extensions of their maxillary artery [40].
Meanwhile, the lower gingiva only accepts blood through a smaller artery called the inferior dental artery, which is a thinner branch of the maxillary artery. The increased blood flow can increase the risk of implantation by circulating tumor cells to the upper gingiva.
Early diagnosis of a gingival mass metastasized from an underlying primary cancer was critical to patient prognosis. However, misdiagnosis or missed diagnosis can result from several factors. First, the low incidence rate and indistinct manifestations (bleeding, swelling, ulceration, etc.) have posed new challenges for physicians to recognize this rare disease. Second, the misleading characteristics of gingival lesions, such as mimicking pyogenic granuloma or botriomycoma [3, 20], would make physicians forget about the need for a biopsy. However, the rapid growth characteristic of a gingival mass may put physicians on alert for a malignancy. As indicated in the present case, the gingival lesion was initially diagnosed as a primary gingival tumor (botriomycoma )until the biopsy and pathological test were completed; then, an HCC metastasis was finally identified [41].
treatments for primary hepatocellular carcinoma involved hepatectomy, chemotherapy, transarterial chemoembolization (TACE), transcatheter arterial embolization (TAE), novel targeted cancer therapy (sorafenib), and combination therapy. Primary treatments for gingival lesions included resection, chemotherapy, radiotherapy, and TAE. The effectiveness of treatment for survival remains to be confirmed on the basis of large sample randomized controlled studies. As an integral part of evidence-based medicine, case reports and literature reviews have profoundly influenced the medical literature, and they continue to advance our knowledge of disease and help generate hypotheses for conducting clinical studies and basic research.
Conclusion
The diagnosis of a metastatic gingival lesion in patients is challenging because to the rarity of this kind of primary liver cancer. Even if no clear clinical presentation is present, a biopsy is necessary to prevent a potential incorrect diagnosis. A timely diagnosis and treatment of early-stage liver cancer or a metastatic gingival lesion may increase the chance of survival.
Consent:
Informed consent was obtained from all participants included in the study.
Conflict of Interest:
The authors declared no conflict of interest.